Rheumatic Pain
Osteopaths are qualified to help with pain caused by rheumatological conditions.
What Are Rheumatological Conditions?
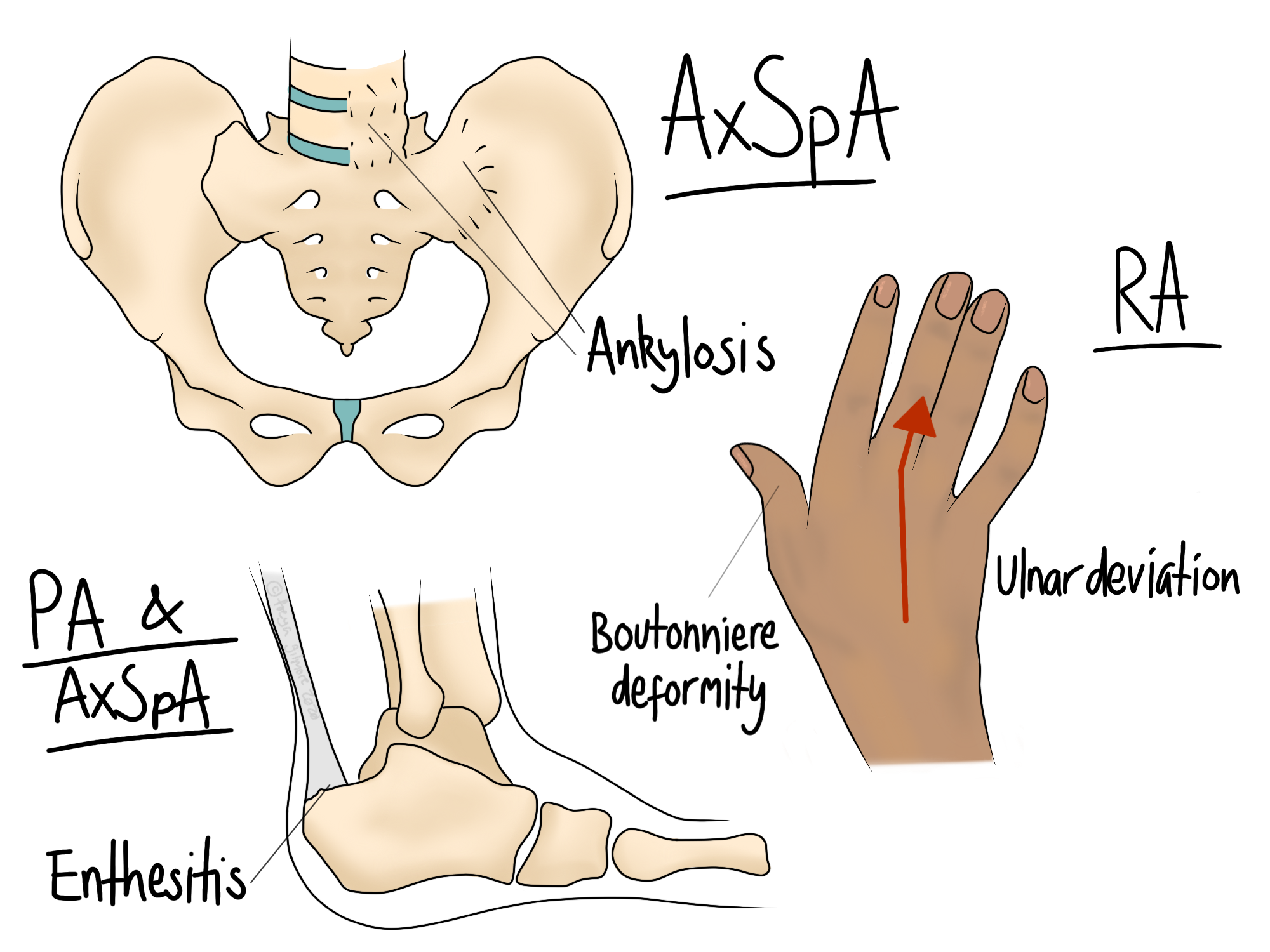
Rheumatology is a broad umbrella that mostly covers autoimmune conditions, as well as conditions that don’t really fit under any other speciality. When an autoimmune condition attacks joints, the symptoms may be particularly responsive to osteopathy. Rheumatoid arthritis, psoriatic arthritis, and ankylosing spondylitis are examples of rheumatological conditions that affect joints.
Fibromyalgia can also be considered rheumatological, although its pathology is unclear. Osteopaths can help with fibro symptoms too.
The Effects on Joints
The exact pathology varies from condition to condition, but when the body attacks its own joints, it’s typically focused on one small part of it. Rheumatoid arthritis (RA) attacks one layer of the joint surface, and ankylosing spondylitis (AS) attacks the point where bone and tendon meet. These episodes of attacking cause damage to the targeted tissue. But sometimes it’s the body’s attempt to heal that is the real problem. After the inflammatory phase of AS has passed, the body lays down new bone over the injury. As AS mainly attacks the spine, this means that bone is laid over the spinal joints, causing gradual stiffening over time. In RA, the small joints of the hands are attacked, and the body’s repairs cause hard “swellings” over the knuckles, and cause the wrist to deviate outward over time.
How Can Osteopathy Help?
We work with achey joints all day, so we’re in a good position to spot when something warrants further investigation. Maybe your joint pain started out like a mysterious sprain, but it has other features that don’t quite add up. We might want to refer you on for blood tests or other investigations if your pain:
follows an inflammatory pattern. It responds well to a cool compress even after the acute phase, it’s worse after rest and relieved by movement.
relapses and remits. Especially if each episode is progressively worse.
as accompanied by other cumulative changes, like a change to posture, lumps on the knuckles, or a change of angle in the wrist.
Some rheumatological conditions can only be diagnosed by a rheumatologist, so referring you back to the GP is the first step in reaching an answer. Sometimes the diagnosis is just a useful label, and sometimes it unlocks medications that can prevent or slow the progression of the disease.
Managing Rheumatic Pain
With a diagnosis in hand, we can work with you to find exactly how much movement your joints want. During an episode, there is usually inflammation around the joint. Movement helps to flush it away, but doing too much can make it more symptomatic once you take a rest. Finding the sweet spot for treatment and for your own self management is key to reducing pain, and potentially the damage done by the disease.
Alongside advice for exercise, we can help you with lifestyle changes and general first aid. How and when to utilise ice or heat, the use of foam rollers, and desk ergonomics are examples of changes that might help.
Make an appointment to manage your rheumatic pain in Flitwick here.